The following is a blog post by our work experience 6th Form student Olivia Barbosa-Atkins.
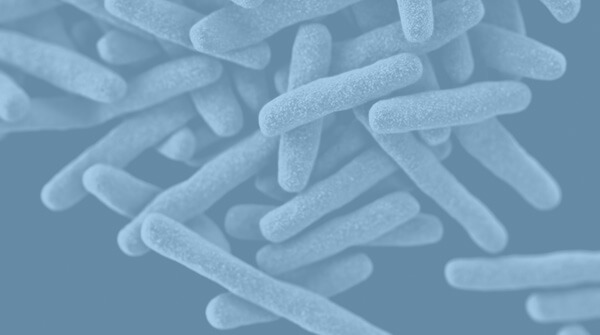
What Is Legionella?
The cause of Legionnaires’ disease is the bacterium Legionella pneumophila. We find Legionella in both potable and non-potable water sources. Legionnaires’ disease (LD) is a grave form of pneumonia typically categorised by the onset of feelings of weakness and fatigue after the incubation period of 2 to 10 days (Legionella.org). Thereafter, the symptoms increase in severity. This ranges from a high temperature of above 39.5°C, violent coughing fits, diarrhoea and often vomiting and headaches. In the monthly legionella report by Public Health England, there have been 346 cases of LD in the UK since 1st January 2017 (as of 4th August 2017). A total of 66 of those cases were reported during July 2017. (gov.uk).
Legionnaires’ Disease Treatment
Treatment for severe cases of LD may take place in the intensive care unit (ICU). For LD sufferers, a stay in ICU would typically entail the patient(s) being attached to ventilators to assist their breathing if they can’t do so on their own and constant monitoring by specially trained nurses and doctors (assisted by monitoring equipment to monitor heart rate, blood pressure, oxygen levels etc). Other equipment includes IV lines and pumps to provide fluids, nutrition and medication, feeding tubes if the patient is unable to eat normally and drains and catheters to remove excess blood and fluid or urine, respectively. (nhs.uk).
Legionnaires’ disease and Post-Traumatic Stress Disorder
Post-traumatic stress disorder (PTSD) is an anxiety disorder that typically develops after a traumatic event or situation. We often associate PTSD with shell shocked soldiers. However, PTSD can develop from any highly distressing incident ranging from serious car accidents to sexual assault.
The link between Legionnaires’ disease and post-traumatic stress treatment in ICU may not be overtly evident on first appraisal. However, the development and subsequent treatment of LD has been linked with the development of PTSD. PTSD can cause long term changes in brain areas implicated in the stress response which includes the amygdala, hippocampus and prefrontal cortex. These changes can then result in intrusive thoughts, hyperarousal, flashbacks, insomnia and night terrors, changes in memory and concentration, and startle responses (Bremner 2006). As the period of an ICU stay can oftentimes be very distressing and overwhelming for the patient, it may trigger the onset of such changes
Legionnaires’ Disease and Post-Traumatic Stress Studies
Links between Legionnaires’ disease and post-traumatic stress are in various studies.
Lettinga et al (2002) published in Clinical Infectious Diseases found a startling link between PTSD and survivors of an outbreak of LD in The Netherlands. The study involved collecting data from questionnaires delivered to 122 of said survivors. The questionnaires were delivered at 2 months and 17 months after antibiotic therapy completion (1st April 1999 for all patients). The first assesses whether the patients had any symptoms associated with LD. Furthermore, it analysed how these symptoms developed in severity over time. Meanwhile, the second, the SF-36, was a 36-item test addressing the eight dimensions believed to reflect the patients’ quality of life. The latter would provide an indication of whether the respondent was suffering from PTSD. The results from this study found that 15% of patients suffered from PTSD after their treatment for LD.
This may not appear to be a significant statistic. However, the percentage of patients with PTSD in this study is in agreement with estimations that, in the aftermath of a disaster, 20-30% of victims develop PTSD.
Conclusions
In conclusion, whilst it is not LD itself which could lead to the development of PTSD; those who are in ICU due to the severity of their symptoms may indeed develop PTSD. Through no fault of the staff, stays in ICU are often traumatic times. Consequently, as with any traumatic experience, this results in PTSD. With this knowledge, health care providers can better implement measures to help those at risk of PTSD following treatment for LD; especially those involved in outbreak situations where media coverage may intensify the trauma. With these precautions, it could be possible to improve the mental wellbeing of those who have suffered through LD.
References
Bremner, J.D. (2006). Traumatic stress: effects on the brain. Dialogues Clin Neurosci 8(4):445–461.
Griffiths, J. (2007). The prevalence of post traumatic stress disorder in survivors of ICU treatment: a systematic review. Intensive Care Medicine 33(9):1506-1518.
Lettinga, K.D (2002). Health-Related Quality of Life and Posttraumatic Stress Disorder among Survivors of an Outbreak of Legionnaires Disease. Clinical Infectious Diseases 35(1):11–17.