Pseudomonas Control
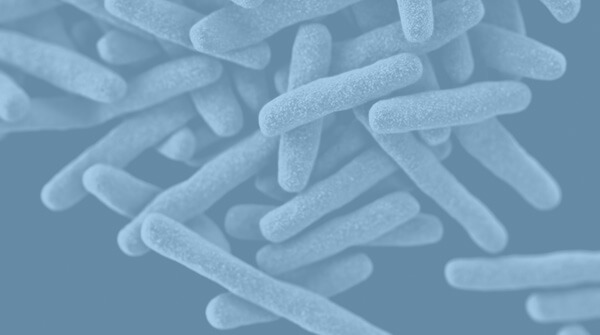
Pseudomonas seldom infects healthy individuals. However, it's a significant threat to those already suffering from a medical condition, particularly cystic fibrosis, AIDS and cancer. It is also very hard to eliminate. Our copper and silver water treatment system is a proven method of Pseudomonas control for commercial sites, industrial buildings and cooling towers.
Pseudomonas Control
Known to be highly resistant to antibiotics, infections cased by P. aeruginosa can unfortunately be very dangerous, in some cases resulting in fatalities. Therefore, it is critical that a proven Pseudomonas control method is in place at industrial and commercial sites.
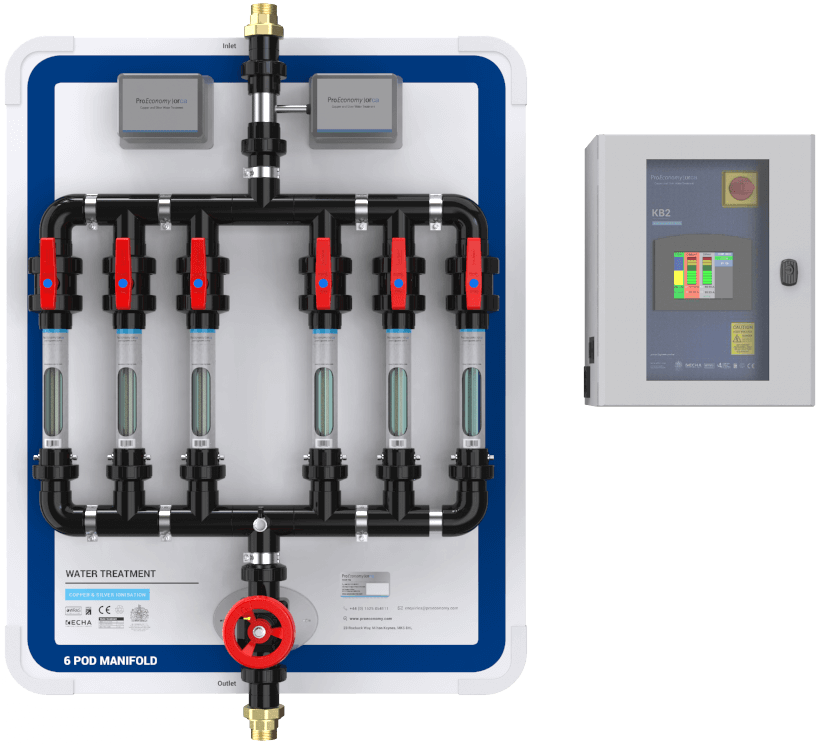
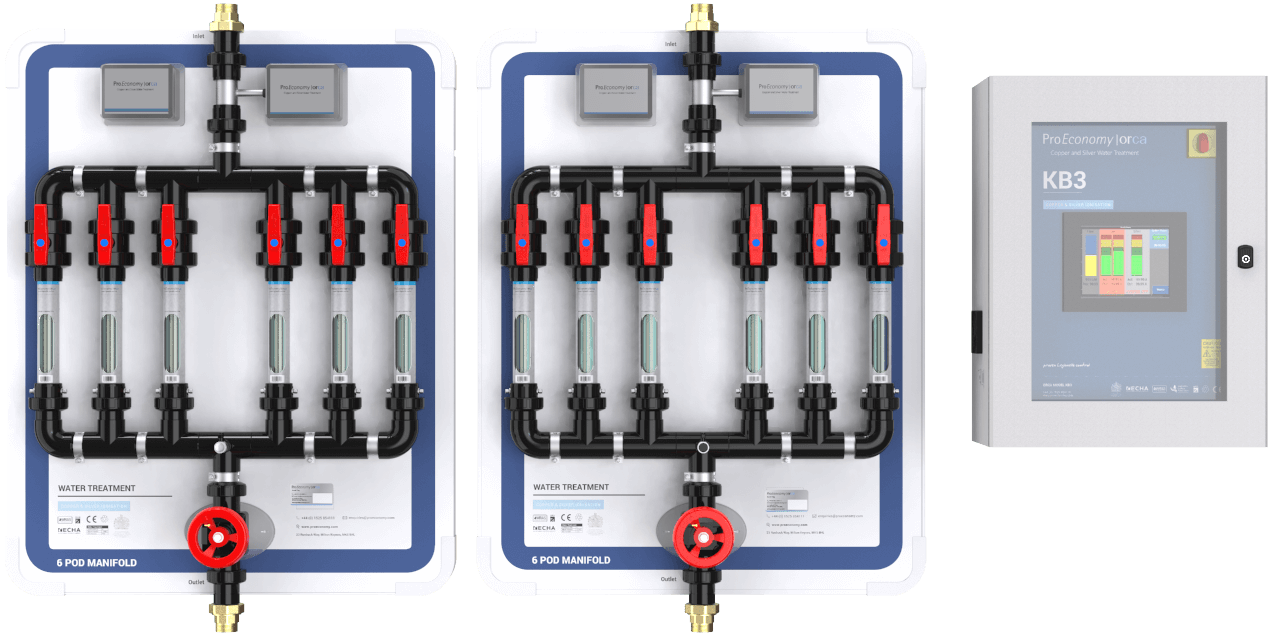
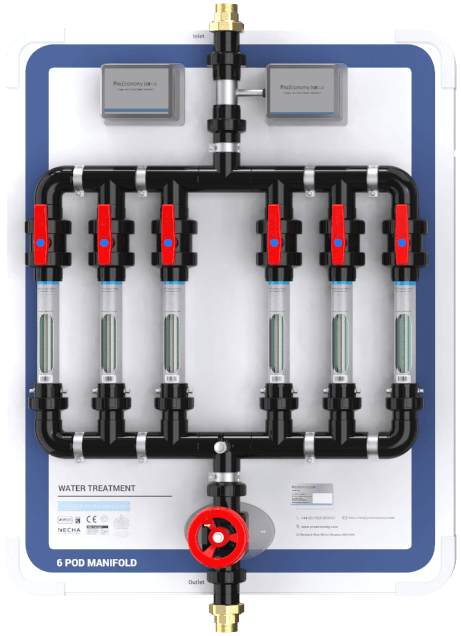
Our Orca copper and silver ionisation system provides advanced Pseudomonas control for cooling towers and industrial and commercial sites across the UK and Europe. Unlike other water management systems, copper silver ionisation contains the following benefits:
- Is non-corrosive
- Has a proven residual effect
- Is fully compliant
- Is scientifically proven to work
- Creates no COSHH issues
- Is effective at high and low water temperatures
The Science Behind Pseudomonas Control With The Orca
Researching water treatment since 1993 has enabled us to build up ample data on Pseudomonas control methods. We are also able to prove the efficacy of the Orca system for Pseudomonas control with case studies and scientific reports.
With a PhD in Legionella control, ProEconomy founder Dr Birgitta Bedford has researched and compiled a list of 40 scientific papers that support copper and silver ionisation for water treatment, some of which you can view here.
Lutz, J.K. & Lee, J., 2011.
Prevalence and antimicrobial resistance of Pseudomonas aeruginosa in swimming pools and hot tubs.
Int. J. Environ. Res. Public Health, 8, 554-564.
"The temperature range in indoor recreational water is ideal for P. aeruginosa proliferation, which routinely grows in water 4-42 degrees Centigrade."
About Pseudomonas
Pseudomonas is a water borne pathogen that typically infects those already suffering from a medical condition. Unfortunately it is regularly found in hospital water supplies hence why Pseudomonas control for healthcare facilities is vital.
Pseudomonas Sampling and Management
Our Tetras, our cloud based water management system uniquely combines our water sampling service and bespoke water management software to provide you with real-time results that allow you to monitor Pseudomonas and control water risk.
Health and Safety Executive, (2014) HSG274 Part 2: The control of bacteria in hot and cold water systems, para. 2, p.3
“There is a reasonably foreseeable Legionella risk in your water system if:
- water is stored or recirculated as part of your system
- the water temperature in all or some part of the system may be between 20–45 °C;
- there are deposits that can support bacterial growth, such as rust, sludge, scale and organic matter;
- it is possible for water droplets to be produced and, if so, if they can be dispersed;
- it is likely that any of your employees, contractors, visitors etc. could be exposed to any contaminated water droplets.”
How Does The Orca Control Pseudomonas?
Percent positive Pseudomonas samples before and after installation of the Orca system at 7 UK hospitals
Hospital 1
A small 40-bed private hospital in the Midlands
% positive Pseudomonas samples
Hospital 2
A small 40-bed private hospital in the Midlands
% positive Pseudomonas samples
Hospital 3
A 900-bed hospital in the west of England
% positive Pseudomonas samples
Hospital 4
A new wing of a large London hospital
% positive Pseudomonas samples
Hospital 5
A 600-bed hospital in the south-east of England
% positive Pseudomonas samples
Hospital 6
A 700-bed hospital in the midlands
% positive Pseudomonas samples
Hospital 7
A 650 bed hospital in the south-east of England
% positive Pseudomonas samples
Scientific Evidence for Pseudomonas Control With Copper and Silver Ionisation
- Field Studies
- Panzer et al. (2013) studied the isomorphic deactivation of a Pseudomonas aeruginosa oxidoreductase. They showed using X-ray crystallography that the silver ion binds to a key respiratory enzyme in P. aeruginosa, inactivating it. Link to abstract
- Fisher et al. (2009) studied the combined effect of copper and silver against Pseudomonas. Sterile cotton swabs impregnated with copper nitrate and silver nitrate solutions removed 100% of P. aeruginosa from a stainless-steel surface. There was no cross-contamination of other surfaces when the wipes were applied, suggesting that the microbes had been inactivated.
- Huang et al. (2008) studied the in-vitro efficacy of copper and silver ions in eradicating Pseudomonas aeruginosa, Stenotrophomonas maltophilia and Acinetobacter baumanii. The three species of bacteria were exposed to a range of copper ion concentrations (0.1 - 0.8 mg/L), silver ions (0.01 - 0.08 mg/L), and combinations of both. All copper solutions achieved more than 99.99% reduction of P. aeruginosa. Silver at 0.04 - 0.08 mg/L achieved more than 99.99% reduction. The two together showed a synergistic effect. Link to paper
- Yahya et al. (1989) demonstrated complete inactivation of Pseudomonas aeruginosa, and a 2.4 log10 reduction within 2 minutes of Staphylococcus species, by 0.4 mg/L copper, 0.04 mg/L silver, and reduced levels of free chlorine (0.3 mg/L).

ProEconomy are members of the copper and silver association.
The copper and silver association is a free open access website that documents scientific publications, peer reviewed papers, reports, policy documents, thesis's and web and magazine articles on copper and silver ionisation and Pseudomonas control.
Visit the Copper and Silver Association website to find out more about Copper and Silver Ionisations efficacy.